FDA expert panel endorses Moderna's COVID-19 vaccine, clearing the way for regulators to greenlight the shot
An independent panel of experts voted on Thursday to recommend that the US authorize Moderna's coronavirus vaccine for emergency use in adults, clearing the way for an imminent regulatory OK of a second COVID-19 vaccine in the US.
Twenty of the 21 committee members voted yes, and one panelist abstained.
US Food and Drug Administration regulators are expected to authorize the shot as soon as Friday, anonymous sources told the New York Times. If the vaccine gets the FDA's regulatory go-ahead, the government plans to ship 5.9 million doses of Moderna's shot to more than 3,000 sites across the nation next week.
A late-stage clinical trial found the shot to be 94% effective at preventing symptomatic COVID-19, which is on par with Pfizer's shot. There were no major safety concerns with the two-dose vaccine, FDA regulators said in briefing documents released Tuesday. There were also no severe cases of COVID-19 among vaccinated study participants, compared with 30 severe cases in the group who got placebo injections.
During an all-day virtual meeting Thursday, a group of leading independent experts discussed and debated the vaccine's application for emergency use authorization. The committee included some of the nation's leading virologists, infectious-disease experts, and clinical researchers.
Advisory committee members and pharmaceutical representatives both stressed the urgency of the situation, noting that one person who got a placebo shot has already died from a severe case of COVID-19, and that there were so many cases during the study period that the trial was wrapped up five months earlier than expected.
"We currently have over 450 cases that are making their way through the adjudication process," Dr. Jaqueline Miller, an infectious disease vaccine development expert with Moderna said, calling it a "tsunami" of new infections.
"Additional severe cases and deaths are a question more of when than a question of if," she said.
3:00 PM: Could Moderna's shot provide some protection after a single dose? It's possible, FDA says
Moderna's COVID-19 vaccine trial was designed to measure how well two shots, given 28 days apart, protect people from infections. And it showed the vaccination works very well at that: it is 94% effective at preventing symptomatic COVID-19, 14 days after a second shot.
But, it's possible that good protection from infection starts much sooner than that.
Preliminary trial data suggests the first dose of Moderna's vaccine likely provides a decent measure of protection from infection all on its own.
Researchers found fewer COVID-19 cases among people who got Moderna's shot compared to the placebo group after volunteers got their first injection, but before they got the second booster dose. That protection appeared to ramp up over time, generally kicking in a couple weeks after the initial shot.
"This could suggest some protection after the first dose, but data is limited by the very short follow-up, around 28 days, as the majority of the study subjects received a second dose," Dr. Rachel Zhang, an FDA medical officer said.
Overall, the single shot appeared to be about 70% effective at preventing symptomatic infections. That looks better than Pfizer's potential one shot protection, which appeared to be about 54% effective in the 21-day period before participants in that trial got a second injection.
Evercore ISI biotech analyst Umer Raffat also pointed out how well Moderna's first dose might work on its own in a recent research note to investors. Data suggests the first dose was about 92% effective compared to a placebo, when looking at first COVID-19 occurrences starting two weeks after the first dose, Raffat said.
It's still unclear how protective one dose would be in the long run, without a second shot. But Raffat, along with a handful of thought leaders in the drug industry like Pfizer board member and former FDA head Scott Gottlieb and University of Pittsburgh researcher Walid Gellad, have advocated the potential benefits after one dose should be considered, especially given the state of the pandemic right now.
Dr. James Hildreth, an immunologist on the committee, and an esteemed HIV researcher, also suggested that since so many people in the US have already had COVID-19, they might receive ample benefit from just one dose of Moderna's vaccine.
"There are probably tens of millions of Americans who've already been infected," Hildreth said Thursday during the meeting. "What I'm asking is, if you took the ones who have been infected, and gave them an injection of your vaccine, could that possibly serve as a boost?"
Moderna's Dr. Jaqueline Miller said that as more study data becomes available in the weeks and months ahead, that could be something to look into.
Operation Warp Speed is holding back half of the available doses to ensure each vaccine recipient gets their booster dose at the right time — after three weeks for Pfizer's shot, and after four weeks for Moderna's.
Gottlieb and Gellad have argued it would be better to distribute all the doses right away, getting a first dose to twice as many people. While this opens up a risk that there may not be enough supply for everyone to get their booster shot on time, they say this could be an acceptable risk to take during the most deadly period of the pandemic.
2:45 PM: One panelist inquires about above-average Bell's palsy rates, but the numbers are too small to draw conclusions
Dr. Paul Offit, a committee member and vaccine expert at the University of Pennsylvania, highlighted that both Moderna's and Pfizer's vaccine studies appeared to have higher rates than usual of Bell's palsy.
Bell's palsy is a typically temporary condition marked by weakness or paralysis in facial muscles. FDA scientists have acknowledged more people getting the coronavirus vaccines developed this condition than those getting placebo.
But the number of cases — seven among more than 30,000 vaccinated volunteers — is too small to say if the vaccine caused these cases. Agency reviewers said the Bell's palsy cases in the studies were in line with typical incidence rates.
Offit also said it's important to not fall victim to "the tyranny of small numbers" and conclude a relationship just yet, saying he is pleased the agency will closely monitor these vaccines going forward.
But Offit questioned the notion that the studies had typical rates of Bell's palsy cases. "I'm just not quite sure how we are so comfortable that this was a background rate," he said.
"If you look at the Pfizer trial, there were four cases of Bell's palsy in a group of 22,000 [vaccinated people] per three months, which works out to about 8 cases per 10,000 per year," Offit said. "If you look at the Moderna trial, it's 3 cases for 15,000 for three months, which also works out to about 8 cases per 10,000 per year."
Combining the two placebo groups together, Offit said those volunteers had about 1.2 cases per 10,000 per year. He said that's roughly in line with the background rate.
FDA medical officer Dr. Rachel Zhang said the agency is looking into this.
"There is still no clear basis upon which to conclude a causal relationship, but we definitely see your point with the two studies combined," she said.
She did not dispute Offit's point that the vaccinated groups seemed to have higher-than-normal rates.
11:00 AM: Moderna pitches plan to immunize placebo volunteers without 'jumping the line'
Moderna has a plan to offer trial volunteers who received placebo shots the actual vaccine, while side-stepping some of the key ethical concerns.
What to do with ongoing placebo-controlled trials during the pandemic has become a top conundrum facing vaccine developers like Pfizer and Moderna. On one hand, researchers want to keep following the placebo group to have high-quality, long-term data to see how these shots work. But ethicists also wonder if studies can, or should, withhold an effective vaccine from volunteers.
Moderna's proposal is to ask participants whether or not they want to know if they got the real vaccine or a placebo. They can choose to remain blinded and in the study, or they can decide to know which arm they were in. Placebo participants who choose to become unblinded are then offered the real vaccine from clinical trial stocks, if they want it. All of those participants would be followed for long-term data.
Tal Zaks, Moderna's chief medical officer, said this would not take doses away from priority groups. Instead, placebo recipients would get doses already produced for the sole purpose of clinical trial use that can't be dispatched to the general public.
"None of our vaccine trial participants would be 'jumping the line' ahead of others, because we have clinical trial supplies available that would in fact expire and go to waste if we don't use them," Zaks told the panel.
Dr. Lindsey Baden, an infectious-disease expert at Brigham and Women's Hospital, also spoke as part of Moderna's presentation as one of the study's investigators.
Baden said there have been a "substantial" number of volunteers dropping out of the trial in the last week since Pfizer's vaccine secured an emergency OK last Friday.
"This dropout undermines the data integrity and what can be learned," Baden said. "We must be proactive to ensure that the best choice is for our participants to remain in the study."
Giving placebo recipients the chance to be vaccinated is important, because Zaks said many of the volunteers are at higher risk of infection and also have risk factors for severe disease.
A 54-year-old man with diabetes who got placebo shots in Moderna's trial ultimately died from COVID-19, Zaks said, highlighting the risk in not immunizing these volunteers.
9:50 AM: FDA and CDC are investigating allergic reactions to Pfizer's vaccine, but have no answers or recommendations yet

Dr. Stanley Perlman, a University of Iowa immunologist, asked about possible explanations for allergic reactions to COVID-19 vaccines, after two healthcare workers in the UK, and then two more in Alaska, had anaphylactic reactions after receiving Pfizer's vaccine.
Pfizer's vaccine ingredients don't seem to be anything highly allergenic, and at least one of the healthcare workers had no history of allergies, leaving experts (like Perlman) puzzled as to what's going on.
"At this point we and CDC are continuing to investigate cases and consider data," said Doran Fink, an FDA vaccine expert. "At this point, we don't have enough information to make definitive recommendations one way or another, and as we continue to investigate and evaluate the data we will consider whether additional recommendations need to be made."
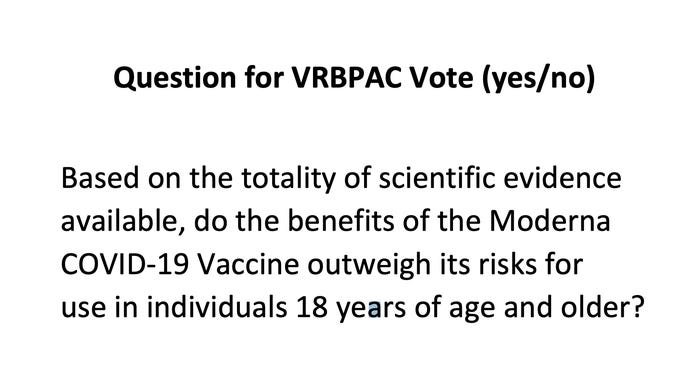
9:00 AM: Panel kicks off, releasing key voting question
We are off and running for a marathon meeting expected to wrap up at 5:15 p.m.
On Tuesday, the FDA released the most detailed results yet from Moderna's late-stage study in preparation for this meeting. The agency's summary showed the two-dose vaccine to be overwhelmingly protective at preventing symptomatic COVID-19 with no major safety concerns.
All in all, it's a very similar profile to Pfizer's vaccine, which was authorized last Friday, and we compared what we know about each shot here.
It's poised to be a long but important day. The panel's recommendation on whether or not to OK Moderna's vaccine is seen as the last remaining barrier to an FDA authorization decision.
Here's the agenda for the day:
9:00 a.m. — Introductions
9:30 a.m. — FDA deputy director Doran Fink outlines emergency use authorization
10:05 a.m. — Stanford researcher Steven Goodman discusses the possible options for ongoing placebo-controlled vaccine trials, given COVID-19 shots are now being rolled out
10:45 a.m. — Moderna chief medical officer Tal Zaks and senior vice president Jacqueline Miller present the biotech's vaccine data
12:00 p.m. — Public comment
1:00 p.m. — Zaks and Miller answer questions from committee members
2:00 p.m. — FDA medical officer Rachel Zhang presents the agency's perspective on the vaccine data
3:10 p.m. — Committee discusses, ultimately votes, and adjourns